Does Cannabis Help Depression? What Research and Clinical Practice Suggest Today


Cannabis has often been discussed as a substance that may influence mood and emotional balance. In some cases, people report feeling calmer or emotionally lighter after using cannabis, while others describe increased anxiety or discomfort. Current research suggests that these mixed experiences may be related to how cannabis interacts with brain systems involved in mood regulation.
However, it has not been established that cannabis can treat depression itself, and available evidence remains limited. This article aims to organize what is currently known, based on research findings and observed patterns in medical settings.
Does Cannabis Help Depression
When people ask whether cannabis helps depression, they are often looking for a clear yes or no answer. However, based on current research and clinical observations, the relationship between cannabis and depression appears to be complex. Cannabis is not considered an established treatment for depression, but it may influence mood-related symptoms in some situations.
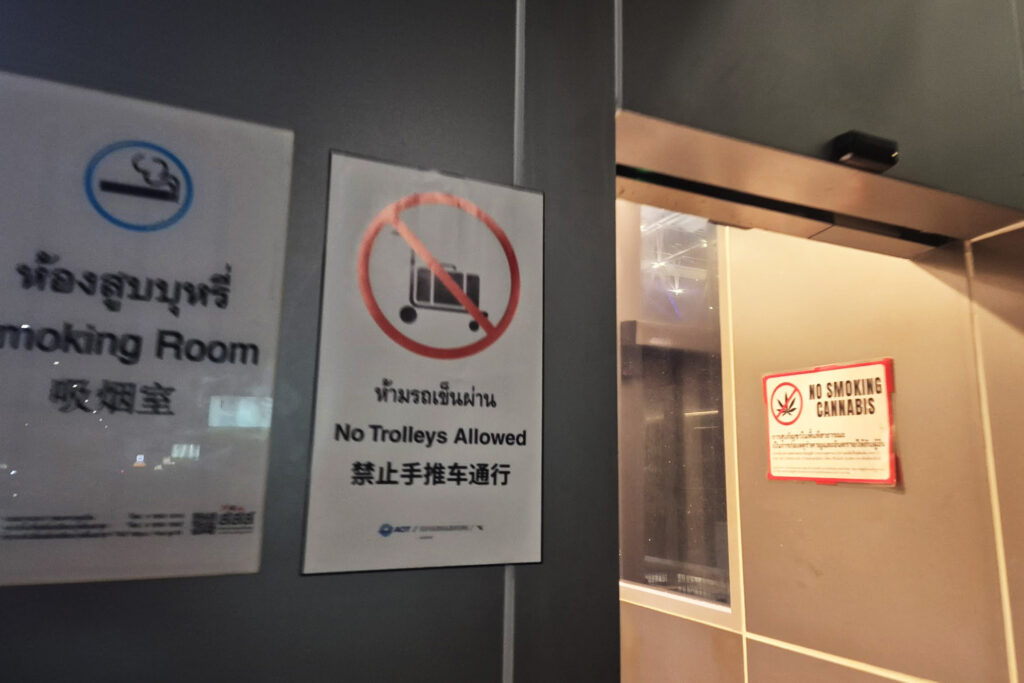
From what I have observed in medical cannabis clinics and dispensaries in Thailand, discussions usually focus on stress relief, emotional tension, or sleep-related concerns rather than direct treatment of depressive disorders. Research institutions also describe cannabis as something that may interact with brain systems involved in mood regulation, while emphasizing that evidence remains limited and inconsistent (According to: National Institutes of Health).
To understand why answers vary so widely, it is first necessary to clarify what “depression” typically refers to in these discussions and why people report very different outcomes after using cannabis.
What “Depression” Usually Refers To in This Context
In many conversations about cannabis, the word “depression” is used broadly. It may refer not only to clinically diagnosed depressive disorders, but also to ongoing low mood, emotional fatigue, stress-related symptoms, or difficulty sleeping. This difference in meaning matters, because research findings depend heavily on how depression is defined.
From what I have heard directly from clinicians in Thailand, cannabis is more often discussed in relation to mood balance, stress reduction, or sleep support rather than as a primary approach for diagnosed depression. Clinical depression is generally understood as a complex condition involving changes in neurotransmitter activity and stress-response systems. Studies suggest that serotonin, dopamine, and the endocannabinoid system may be involved in these processes, although the exact mechanisms are still being studied (According to: National Institutes of Health).
Because of this, experiences described as “relief from depression” may reflect temporary changes in stress levels or emotional tension rather than direct effects on the underlying condition itself.
Why People Report Opposite Experiences
Another reason this topic is often confusing is that individual responses to cannabis appear to vary widely. Factors such as brain chemistry, current emotional state, dosage, and cannabinoid balance may all influence how cannabis is experienced. Some people describe feeling calmer or mentally lighter, while others report increased anxiety or emotional discomfort.
Research has suggested that THC may temporarily elevate mood in some individuals, while in others it may intensify anxiety or physical stress responses, particularly at higher doses (According to: National Institutes of Health). Environmental factors such as setting, expectations, and existing stress levels may also shape these outcomes.
Based on what clinicians and dispensary staff commonly explain, this variability is one reason cannabis is approached cautiously in mental health contexts. Rather than producing a predictable effect, cannabis appears to interact with existing emotional states, which helps explain why reports about its impact on depression can seem contradictory.
How Cannabis May Affect Mood and Stress Response
Research suggests that cannabis may interact with biological systems involved in mood and stress regulation. Rather than acting as a direct antidepressant, cannabis appears to influence how the brain responds to stress, emotional stimuli, and internal balance. This interaction is thought to occur through multiple pathways, including the endocannabinoid system and neurotransmitters related to emotional regulation.
From what I have heard repeatedly from medical professionals in Thailand, cannabis is often discussed as something that may alter stress perception or emotional tension, rather than as a treatment aimed at correcting depression itself. To understand these effects more clearly, it is useful to look at the underlying systems that are commonly mentioned in research.
The Endocannabinoid System and Mood Regulation
The endocannabinoid system, often referred to as the ECS, is a biological system involved in maintaining internal balance within the body. It plays a role in processes such as stress response, emotional regulation, sleep, and appetite. Researchers have suggested that the ECS may help the body adapt to stress and emotional strain.
Cannabis-derived compounds, such as THC and CBD, are known to interact with cannabinoid receptors that are part of this system. Studies indicate that this interaction may influence how the brain processes stress or emotional signals, although the exact mechanisms are still being studied (According to: National Institutes of Health).
Based on clinical explanations I have heard, this ECS interaction is one reason cannabis is sometimes associated with feelings of relaxation or emotional relief. At the same time, because the ECS functions differently in each individual, these effects are not consistent or predictable.
Neurotransmitters Often Mentioned in Depression Research
Depression research frequently focuses on neurotransmitters such as serotonin and dopamine, which are involved in mood regulation, motivation, and emotional processing. Changes in the activity of these neurotransmitters are commonly discussed in relation to depressive symptoms.
Some studies suggest that cannabis may indirectly influence neurotransmitter activity through its interaction with the ECS and stress-response pathways. For example, cannabinoid signaling has been associated with changes in serotonin-related receptors and dopamine pathways in certain experimental settings (According to: Harvard Medical School).
However, researchers also emphasize that these findings do not mean cannabis corrects neurotransmitter imbalances in the same way as established medical treatments. The observed effects appear to be complex, context-dependent, and influenced by dosage, timing, and individual sensitivity.
Why High THC May Increase Anxiety in Some People
While some people report feeling relaxed after using cannabis, others experience increased anxiety, restlessness, or physical discomfort. One factor often mentioned in research is THC concentration. Higher levels of THC have been associated with a greater likelihood of anxiety-related responses in some individuals.
Studies suggest that THC may stimulate stress-related pathways in the brain at higher doses, potentially increasing heart rate or emotional sensitivity rather than reducing stress (According to: National Institutes of Health). This response appears to vary depending on individual brain chemistry, emotional state, and environmental context.
From what dispensary staff and clinicians in Thailand frequently explain, this dose-dependent effect is one reason caution is often advised, especially for people who are already experiencing emotional instability or high stress. Rather than producing uniform calming effects, high-THC products may amplify existing anxiety in certain situations.
What Research Suggests So Far
Research on cannabis and depression has increased in recent years, but the overall findings remain cautious and limited. Rather than showing clear treatment effects, many studies describe potential mechanisms or early signals that require further confirmation. At this stage, research tends to focus on how specific cannabinoids may influence anxiety, inflammation, and mood-related pathways, rather than proving clinical effectiveness.
Medical professionals I have spoken with often emphasize that current evidence should be understood as exploratory. To see what has been observed so far, it is helpful to separate findings related to CBD, THC, and early experimental studies.
CBD and Potential Links to Anxiety and Inflammation Pathways
CBD has received attention in research due to its non-intoxicating nature and its possible interaction with stress-related biological systems. Studies suggest that CBD may influence receptors involved in serotonin signaling and inflammatory responses, both of which are often discussed in relation to anxiety and mood regulation. This has led researchers to explore CBD’s potential role in reducing stress-related symptoms.
Some experimental and early clinical studies have reported that CBD administration was associated with reduced anxiety measures in specific settings. Researchers have also noted possible anti-inflammatory effects that could indirectly influence emotional well-being (According to: University of São Paulo Research Team).
However, these findings do not establish CBD as a treatment for depression. Reported effects vary widely, and questions remain regarding appropriate dosage, duration of use, and long-term outcomes.
THC and Mood Effects: Possible Benefits and Known Risks
THC has been studied for its psychoactive effects, including changes in mood and emotional perception. Some research suggests that low doses of THC may temporarily elevate mood or reduce perceived stress in certain individuals. This has led to discussion about possible short-term mood benefits.
At the same time, research consistently notes that THC may also increase anxiety, paranoia, or emotional instability, particularly at higher doses or in vulnerable individuals (According to: National Institutes of Health). These opposing effects are one reason THC-related findings are often described as dose-dependent and highly individual.
Because of this dual nature, researchers and clinicians generally caution against viewing THC as a reliable approach for managing depressive symptoms.
Animal Studies and Early Human Evidence
Animal studies have been used to explore how cannabinoids might influence behaviors associated with depression. Some experiments have reported reductions in depression-like behaviors following cannabinoid exposure. These findings have been cited as early indicators of potential antidepressant-like effects. (According to: McGill University Research Team)
In addition, a small number of early human studies have observed improvements in anxiety or mood-related measures after CBD use. However, most of these studies involve limited participant numbers and short observation periods. As a result, researchers generally agree that current evidence is insufficient to draw firm conclusions about effectiveness in depression.
Based on both published research and clinical commentary, the prevailing view is that these findings are promising but preliminary, and that much larger and longer-term studies are required.
Why Some People Feel Temporary Relief
Even though cannabis is not considered an established treatment for depression, some people report feeling temporary emotional relief after use. These experiences are often described in terms of improved sleep, reduced physical tension, or a brief sense of mental ease. Such effects appear to be related to short-term changes in stress perception and bodily sensations rather than long-term changes in depressive conditions.
From what I have observed through conversations with users and clinicians in Thailand, these reports tend to focus on how people feel shortly after use, rather than on sustained improvement over time. Understanding the specific experiences involved can help explain why relief is sometimes reported.
Sleep Changes and Short Term Emotional Relief
Sleep disturbance is commonly mentioned by people who experience low mood or emotional exhaustion. Some individuals report that cannabis use makes it easier to fall asleep or reduces nighttime restlessness. Improved sleep quality may temporarily ease emotional strain and make daily stress feel more manageable.
Research has suggested that cannabinoids may influence sleep-related processes, including sleep onset and perceived restfulness, although results vary across studies (According to: National Institutes of Health). When sleep improves, even briefly, people may feel less overwhelmed or emotionally tense the following day.
At the same time, others report disrupted sleep or increased alertness, particularly with higher THC exposure. This variability highlights why sleep-related relief is often described as short term and inconsistent.
Appetite, Body Sensations, and Perceived Calm
Another commonly reported experience involves changes in appetite and bodily comfort. Some people describe feeling physically more relaxed, with reduced muscle tension or digestive discomfort. For individuals whose low mood is accompanied by physical stress or loss of appetite, these bodily changes may feel emotionally relieving.
Research has noted that cannabinoids can influence appetite regulation and sensory perception, which may contribute to a temporary sense of comfort or calm (According to: National Institutes of Health). When physical discomfort decreases, emotional burden may also feel lighter for a short period.
However, these effects do not occur uniformly, and some individuals experience nausea, discomfort, or heightened bodily awareness instead. This range of responses reinforces the idea that perceived relief is closely tied to individual sensitivity.
Reduced Rumination and the “Mental Space” Effect
Some people describe a reduction in repetitive or intrusive thoughts after using cannabis. This is sometimes referred to as a sense of mental space, where constant worrying or overthinking temporarily subsides. For those who tend to ruminate, this pause in mental activity may be experienced as emotional relief.
Researchers have suggested that cannabis may alter attention and emotional processing in ways that shift focus away from persistent negative thoughts, although these effects are not well understood and appear to be short lived (According to: National Institutes of Health).
Based on personal observation, this mental shift does not necessarily resolve underlying emotional difficulties. Instead, it may provide a brief period of rest from ongoing mental strain. As with other reported effects, individual differences play a significant role in whether this experience is perceived as helpful or uncomfortable.
Why Cannabis Is Not an Established Treatment for Depression
Despite growing interest in cannabis and mental health, it is not regarded as an established treatment for depression. Research findings and clinical practice both suggest that current evidence does not support cannabis as a reliable or standardized therapeutic option. The main reasons relate to limitations in existing studies, potential risks for certain individuals, and the cautious stance taken by medical institutions.
Understanding these factors helps clarify why cannabis is generally discussed as a possible adjunct or exploratory option rather than a primary treatment for depressive disorders.
Evidence Limits: Small Samples and Lack of Long Term Data
One major limitation in cannabis research is the size and duration of available studies. Many investigations into cannabinoids and mood involve small participant numbers or short observation periods. This makes it difficult to determine whether observed effects are consistent, durable, or applicable to broader populations.
Long-term studies examining sustained use, relapse rates, or functional outcomes in people with depression remain limited. Research organizations frequently note that without larger and longer trials, conclusions about safety and effectiveness cannot be drawn with confidence (According to: National Institutes of Health).
Because of these gaps, medical guidelines generally refrain from recommending cannabis as a treatment for depression.
Worsening Anxiety, Panic, and Mood Instability in Some Cases
Another reason for caution is that cannabis use does not always lead to symptom relief. Some individuals report increased anxiety, panic reactions, or emotional instability, particularly when using products high in THC. These responses suggest that cannabis may aggravate certain symptoms rather than reduce them.
Research has described dose-dependent effects of THC, where higher exposure is associated with elevated stress responses and emotional discomfort in susceptible individuals (According to: Centre for Addiction and Mental Health). This variability makes it difficult to predict who may benefit and who may experience negative outcomes.
Such risks contribute to the view that cannabis cannot be considered a broadly safe or uniform option for people with depression.
Why Clinics Remain Cautious
In clinical settings, cannabis is often approached conservatively. From what I have heard directly from medical professionals, concerns commonly include insufficient safety data, uncertainty about interactions with prescribed medications, and large individual differences in response. These factors limit the ability of clinicians to recommend cannabis with confidence.
Organizations involved in public health and mental health research emphasize that treatments should be supported by consistent evidence and clear risk profiles. At present, cannabis does not meet these criteria for depression management (According to: World Health Organization).
As a result, many clinics view cannabis, at most, as a potential supplementary option in carefully selected situations rather than a primary or standardized treatment approach.
Key Safety Considerations Before Trying Cannabis
When considering cannabis in the context of depressive symptoms, safety is an essential concern. Experiences reported by users and clinicians suggest that outcomes can vary widely depending on individual conditions, product composition, and usage context. For this reason, cannabis is generally discussed with caution, especially for people already receiving treatment for mental health conditions.
Medical professionals often emphasize that understanding potential risks and limitations is just as important as understanding possible effects. The following points reflect safety considerations commonly raised in clinical discussions.
Do Not Stop Prescribed Treatment Without Medical Guidance
One of the most frequently emphasized warnings from healthcare providers is the risk of discontinuing prescribed treatment without professional supervision. Some individuals report feeling temporarily better after using cannabis and may consider stopping antidepressant or anti-anxiety medication on their own. This approach is widely regarded as risky.
Research organizations note that abrupt discontinuation of prescribed psychiatric medication may increase the risk of withdrawal symptoms or symptom relapse (According to: National Institute of Mental Health). Because cannabis has not been established as a replacement for evidence-based treatments, clinicians generally advise against using it as a substitute.
From what I have heard in clinical settings, cannabis is typically discussed as a possible adjunct rather than an alternative, and only within the context of ongoing medical care.
Why High THC Products Are Higher Risk
THC concentration is another key factor affecting safety. Higher THC products are more likely to produce strong psychoactive effects, which some individuals experience as anxiety, panic, or emotional discomfort. These responses appear more common at higher doses and in people with existing mood instability.
Studies have reported that elevated THC exposure may intensify stress responses, increase heart rate, and heighten anxiety in certain individuals (According to: Centre for Addiction and Mental Health). Because of this, medical professionals often caution against high-THC products for people who are sensitive to anxiety or emotional fluctuations.
This risk profile is one reason why dosage and cannabinoid balance are frequently discussed in medical cannabis consultations.
A Cautious Starting Approach: CBD Dominant, Low Dose, Calm Setting
When cannabis is considered, clinicians often recommend a cautious approach. This typically includes choosing products with higher CBD content, using very low doses, and ensuring a calm and familiar environment. Such conditions may reduce the likelihood of adverse emotional reactions.
CBD has been studied for its potential calming effects without the strong psychoactive impact associated with THC, which is why it is often suggested as a starting point (According to: National Institutes of Health). A quiet and supportive setting may also help limit stress-related responses during use.
Based on observations shared by healthcare providers, this cautious framework does not guarantee positive outcomes, but it may help reduce risk when individuals choose to explore cannabis-related options.
How Medical Cannabis Is Used in Thai Clinical Settings
In Thailand, medical cannabis is generally positioned as a supplementary option rather than a central treatment for mental health conditions. Based on what I have observed through clinic visits and conversations with physicians, cannabis is discussed within a controlled medical framework that prioritizes existing treatment plans. Its use is typically framed around symptom support, not as a replacement for established psychiatric care.
To understand how cannabis is applied in practice, it is helpful to look at the situations in which it is most commonly discussed and the guidance that accompanies its use.
Common Use Cases: Mild Anxiety and Sleep Problems
In clinical settings, medical cannabis is most often mentioned in relation to mild anxiety, stress-related tension, or sleep disturbances. Physicians I have spoken with frequently explain that cannabis is not intended for severe depressive disorders, but may be considered when symptoms are relatively mild and other treatments have not caused significant improvement. Sleep support and stress reduction are the most commonly cited contexts.
Some clinicians describe the use of CBD-dominant products or low-dose THC options to support sleep onset or reduce nighttime restlessness. Research institutions have reported that cannabinoids may influence sleep-related processes, although effects appear to vary widely between individuals (According to: National Library of Medicine).
Importantly, physicians often emphasize that outcomes differ and that cannabis is not presented as a universal solution. Its use is typically limited to carefully selected cases and monitored alongside other treatments.
Medical Certificates and Typical Clinical Advice
Thai medical cannabis clinics generally require a medical consultation before use. During this process, physicians may issue a Medical Cannabis Certificate that documents symptoms, recommended product types, and usage considerations. This certificate serves both as clinical guidance and as documentation of supervised use.
From what I have experienced, clinical advice commonly includes starting with very low doses, avoiding high-THC products, and discontinuing use if adverse reactions occur. Physicians also tend to stress the importance of not altering prescribed psychiatric medication without consultation.
Public health authorities in Thailand have outlined these cautious practices to ensure patient safety and responsible use within the medical system (According to: Ministry of Public Health Thailand).
What We Can Say Today: Balancing Possibility and Caution
After reviewing research findings, clinical perspectives, and real-world observations, it becomes clear that the relationship between cannabis and depression cannot be reduced to a simple conclusion. Current evidence suggests the existence of potential effects, while also highlighting significant uncertainty and risk.
Rather than asking whether cannabis “works” for depression, a more accurate question may be how it is currently understood, where its limits lie, and what considerations are necessary for safer decision making.
Potential Effects Exist, But Treatment Claims Are Not Confirmed
Studies have suggested that cannabinoids such as CBD and THC may influence mood, stress perception, and sleep-related processes. Some individuals report temporary emotional relief, and early research has identified biological pathways that could explain these experiences. However, these findings do not confirm cannabis as a treatment for depression.
Major research institutions consistently describe the current state of evidence as preliminary. While some mechanisms appear promising, results remain inconsistent, and long-term clinical effectiveness has not been established (According to: National Library of Medicine). This gap between observed effects and confirmed treatment outcomes is a key reason why medical guidelines remain cautious.
Based on both research and clinical commentary, cannabis is better understood as a substance that may influence certain symptoms under specific conditions, rather than as a solution for depressive disorders.
Practical Next Steps for Safer Decision Making
Given the uncertainty surrounding cannabis and depression, cautious and informed decision making is essential. This includes maintaining ongoing medical treatment, understanding individual sensitivity, and avoiding unrealistic expectations.
Health authorities and clinicians commonly emphasize the importance of professional guidance, especially for individuals already receiving psychiatric care (According to: World Health Organization). Seeking accurate information, starting conservatively if cannabis is considered, and prioritizing safety over experimentation are often recommended principles.
At present, balancing possibility with caution appears to be the most responsible approach. Understanding both what is known and what remains uncertain allows individuals to make choices that minimize risk while remaining grounded in current evidence.